
Heart Attack, Stroke Risk May Be Elevated Following Cancer Diagnosis
August 25, 2017, by NCI Staff
A diagnosis of cancer can come with an increased risk of a heart attack or stroke in the months following the diagnosis, findings from a new study suggest. Within 6 months of a cancer diagnosis, in fact, the risk of having either event was more than twice that seen in people without cancer.
The risk increases, however, were not evenly distributed. People with lung cancer or with more advanced cancers had the greatest excess risk of stroke or heart attack, Babak Navi, M.D., of Weill Cornell Medicine, and his colleagues reported August 22 in the Journal of the American College of Cardiology.
That people with cancer have an increased risk of events caused by artery blockages—or arterial thromboembolism—is not necessarily a new finding, the researchers wrote. But the study is the first to analyze the issue on a population-wide scale to better clarify the potential scale of the problem and whether there are important differences in risk by cancer type and stage.
The findings raise important issues about the care of people with a new cancer diagnosis, Dr. Navi said.
“Especially now that cancer treatments have improved and long remissions and cures are becoming more common, treating doctors need to work with their patients to focus on not just surviving their cancer but also surviving with a good quality of life,” Dr. Navi said. That means “preventing secondary complications of their cancer, including arterial thromboembolism.”
Recognizing the Risk
The number of people in the United States undergoing active treatment for a cancer is large, 13 million, and is only expected to increase.
People undergoing cancer treatment are known to have a substantially increased risk of developing blood clots in their veins (venous thromboembolism), particularly in the legs and lungs.
Several factors influence this risk, the researchers wrote, including that cancer patients often undergo invasive procedures that can dislodge a clot and that tumors and cancer therapies can affect processes that influence the formation of clots, like coagulation and platelet function.
Oncologists already consider the risk of venous thromboembolism when treating patients, Dr. Navi noted. There is a score that clinicians use when patients are starting chemotherapy to identify those who are at increased risk of these events. And clinical trials have tested therapies to reduce the chance of such events in people at high risk.
The risk of arterial thrombotic events like strokes and heart attacks, on the other hand, has been underappreciated, he said.
In an accompanying editorial, Edward T.H. Yeh, M.D., and Hui-Ming Chang, M.D., M.P.H., of the Center for Precision Medicine at the University of Missouri, agreed that other health concerns can take a back seat once somebody is diagnosed with cancer.
For those undergoing active treatment for cancer, “their primary medical providers are [their] oncologists, cancer surgeons, or radiation oncologists,” Drs. Yeh and Chang wrote.
For these clinicians, their focus and goal is to treat their patients’ cancers, they continued, and “little attention is paid” to managing other health conditions, including diabetes and high cholesterol, that can increase the risk of heart attack and stroke.
Lung Cancer, Advanced Cancers Riskiest
To conduct the study, Dr. Navi and his colleagues used NCI’s Surveillance, Epidemiology, and End Results–Medicare Linked Database. They identified nearly 280,000 people diagnosed between 2002 and 2011 with one of the five most common solid tumors; with non-Hodgkin lymphoma, the most common blood cancer; or with two cancers known to be associated with an increased risk of venous thromboembolism. Each person with cancer was matched with a “control” Medicare patient who did not have cancer.
Using diagnosis codes from medical records, the researchers then identified all cases of ischemic stroke and heart attack that occurred among study participants through 2012.
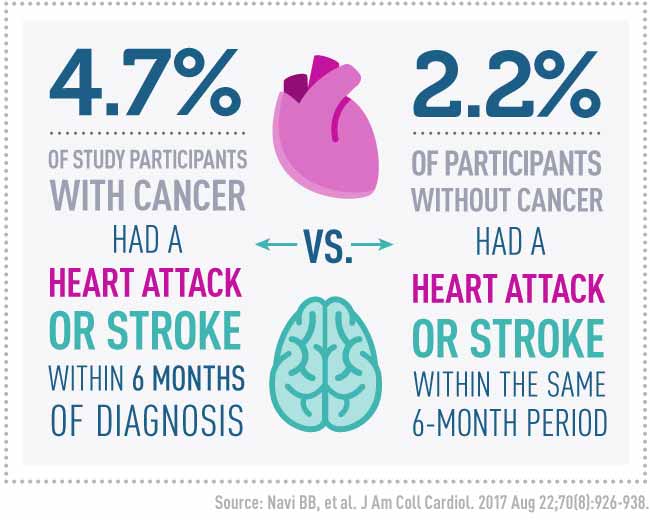
Overall, 4.7% of those with cancer had experienced either a heart attack or a stroke within 6 months of their diagnosis, whereas only 2.2% of those in the control group experienced one of these outcomes within 6 months of diagnosis of cancer in the corresponding case patient.
By far, people with lung cancer had the highest risk of a heart attack or stroke, they reported, with 8.3% experiencing either event within 6 months of diagnosis compared with 2.4% of those in the control group.
By contrast, there was a much smaller difference in risk at 6 months for those with breast cancer (4.2% versus 3.8%) and no difference in 6-month risk for those with prostate cancer (3.9% in both groups).
How advanced patients’ cancers were was also associated with risk of heart attack or stroke, with the risk increasing in parallel with cancer stage. Overall, for example, 3% of those with a stage 1 cancer had an event within 6 months of diagnosis, compared with nearly 8% of those with a stage 4 cancer.
The excess risk of a heart attack or stroke in those with cancer began to diminish after 6 months, the study showed, and by 1 year after diagnosis it had almost entirely disappeared.
Better Assessing Stroke, Heart Attack Risk
Dr. Navi said he was not surprised to see that people with more advanced disease had a greater risk of heart attack or stroke. From a biological perspective, he explained, the observations makes sense because tumors can release enzymes and proteins that can create an environment in which blood clots are more likely to form.
And, he added, “It’s no shock that the highest risk is in patients whose cancer is poorly controlled, because either their treatment hasn’t started or their disease is resistant to treatment,” he said.
The larger excess risk in patients with lung cancer is also to be somewhat expected, said Lori Minasian, M.D., deputy director of NCI’s Division of Cancer Prevention and chair of the institute’s Community Oncology Cardiotoxicity Task Force, which coordinates NCI-supported research on the cardiac effects of cancer treatments.
Many of the risk factors for lung cancer overlap with those for cardiovascular disease, and some therapies commonly used to treat lung cancer can damage the heart, she said.
From a broader perspective, multiple factors could influence arterial thromboembolism risk in people with cancer, Drs. Yeh and Chang wrote. The fact that the increased risk largely resolves within a year suggests that it could be a byproduct of the cancer itself, with successful treatment eventually diminishing the risk, they speculated.
Other evidence points to treatments themselves as important contributors, they added. For example, the targets of many targeted cancer therapies also play a role in maintaining the proper functioning of the cardiovascular system.
From this single study, Dr. Minasian said, it’s difficult to draw conclusions about the factors that may contribute to increased arterial thromboembolism risk in people undergoing cancer treatment and how important the issue is for different patient populations. But, she added, there are some guiding principles that can help oncologists better assess the risk.
“In thinking about this globally, you can divide the assessment into three categories,” she said. “A patient’s baseline cardiovascular risk factors, the stage of their cancer, and the risks for these events posed by the patient’s cancer treatment.”
In those with breast and prostate cancer, for example, even older patients had a low risk in general of a stroke or heart attack. In these cases, Dr. Minasian said, “a patient’s individual comorbidities may be the driver of their risk.”
The new findings are important, she said. Nevertheless, she added, more data is needed on the extent to which patients’ underlying health factors can interact with their tumor and different cancer therapies to influence heart attack and stroke risk.


















.png)










No hay comentarios:
Publicar un comentario