
Trastuzumab Emtansine Improves Survival in Previously Treated Metastatic HER2-Positive Breast Cancer
June 14, 2017, by NCI Staff
Final results from two international randomized trials confirm that trastuzumab emtansine (Kadcyla®) improves survival for patients with metastatic breast cancer that overexpresses the HER2 protein.
Trastuzumab emtansine, an antibody–drug conjugate commonly abbreviated as T-DM1, improved overall survival for women and men with HER2-positive metastatic breast cancer that had progressed after treatment with other HER2-targeted drugs.
"T-DM1 improves both progression-free survivaland overall survival after many lines of therapy in the metastatic setting, which we don't often see with new breast cancer therapies," said Roisin Connolly, M.D., of the Johns Hopkins Kimmel Cancer Center, who was not involved in either trial. "Also, it's really quite well tolerated in terms of side effects. We like this type of drug, because patients not only live longer but also can have a better quality of life than with other standard therapies," she added.
Results from the two clinical trials, called TH3RESA and EMILIA, were published May 16 in The Lancet Oncology.
Consistently Superior Survival
Tumors that overexpress the HER2 protein make up about 20% of all breast cancer cases, occur in both women and men, and are particularly aggressive. Drugs that target HER2, such as trastuzumab (Herceptin®), lapatinib (Tykerb®), and pertuzumab (Perjeta®), have helped close the survival gap for these patients.
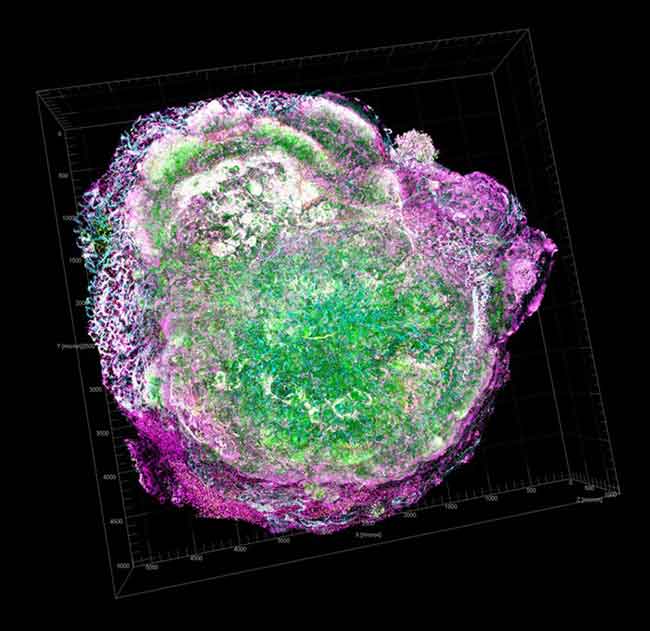
Most HER2-targeted drugs are antibodies or small molecules that bind to and interfere with the function of the HER2 protein, killing cancer cells that rely on HER2 to promote their growth. In contrast, T-DM1 is an antibody–drug conjugate. It uses a molecule of trastuzumab like a homing beacon to carry a toxin, emtansine, directly to cells that overexpress HER2. This delivery mechanism aims to maximize the amount of toxin that reaches cancer cells while minimizing damage to normal cells.
Initial results from the EMILIA trial led the Food and Drug Administration (FDA) to approve T-DM1 for patients who have previously received treatment with trastuzumab and taxane chemotherapy.
EMILIA enrolled 991 patients whose breast cancer had progressed after treatment with both trastuzumab and a taxane. Participants were randomly assigned to receive either T-DM1 or a combination of lapatinib and the chemotherapy drug capecitabine (Xeloda®).
The final results confirmed earlier data from the trial. Patients given T-DM1 had longer median overall survival than patients in the control group—29.9 months, versus 25.9 months for those treated with lapatinib plus capecitabine.
TH3RESA took T-DM1 further down the treatment pipeline, explained Ian Krop, M.D., Ph.D., an oncologist at the Dana-Farber Cancer Institute, who led the trial. "This was the first large trial to look at patients whose cancer had progressed on the HER2-targeted therapies [available] at the time—both trastuzumab and lapatinib," he explained.
In TH3RESA, 602 patients who had progressed after receiving both HER2-targeted drugs and a taxane were randomly assigned to receive either T-DM1 or their physician's choice of third-line treatment, which varied among participating centers.
Again, T-DM1 proved superior; patients receiving T-DM1 had a median overall survival of 22.7 months, compared with 15.8 months for patients receiving other third-line therapy. This survival advantage was seen even though almost half of patients in the control group crossed over to receive T-DM1 after their cancer progressed again.
The EMILIA trial also saw about a quarter of patients in the control arm immediately cross over to T-DM1 after it became clear in analyses part way through the trial that patients receiving T-DM1 lived longer.
In both trials, fewer serious side effects occurred in patients receiving T-DM1. The most common serious side effects seen in TH3RESA participants receiving T-DM1 were thrombocytopenia and hemorrhage.
Making Use of a Cellular Addiction
Before these two trials, "there was a concern based on some laboratory and clinical studies that, after a cancer had progressed on HER2-targeted therapy, the cancer would lose HER2 expression and, therefore, become immune to further therapies targeting HER2," said Dr. Krop. "The data from TH3RESA showed that, at least in a substantial fraction of patients, that's not true.
"That's good news because we can be reasonably confident that, if we develop additional HER2-directed therapies, those are going to have benefit as well," he continued.
HER2 has joined ALK in some lung cancers and BCR-ABL in chronic myeloid leukemia in the category of cancer genes and proteins that remain good treatment targets even after disease progression, explained Dr. Krop.
"I think the common theme among all of these targets is that they are really strong drivers of these cancers," he said. "It's hard for a cancer to lose one [of these targets]…because they're so addicted to the signaling that comes out of these molecules."
This addiction makes it likely that T-DM1 will also be effective for breast cancer patients who receive pertuzumab earlier in treatment, he explained. Pertuzumab, which was not approved by FDA at the time of the TH3RESA trial, is now part of first-line therapy for many patients with newly diagnosed HER2-positive breast cancer.
However, ongoing clinical trials are currently examining this question, "and this is clearly an area where we need to get better data, because right now it’s very limited," he concluded.



















.png)









No hay comentarios:
Publicar un comentario